Who Enforces HIPAA? A Comprehensive Guide to Healthcare Privacy Protection


Introduction
The shift toward digital healthcare has made protecting patient information a mission-critical responsibility. The Health Insurance Portability and Accountability Act (HIPAA) stands as the cornerstone of healthcare privacy protection in the United States, but many healthcare professionals and organizations still wonder: who actually enforces HIPAA regulations?
Understanding HIPAA enforcement is crucial for healthcare providers, insurers, and business associates who handle protected health information (PHI) daily. The consequences of non-compliance can be severe, ranging from hefty financial penalties to criminal charges. This comprehensive guide will explore the enforcement mechanisms, regulatory bodies, and compliance strategies that keep our healthcare system accountable.
HIPAA Compliance Enforcement in Healthcare
The primary responsibility for HIPAA enforcement falls under the U.S. Department of Health and Human Services (HHS), specifically through its Office for Civil Rights (OCR). The OCR serves as the main regulatory watchdog, investigating complaints, conducting audits, and imposing penalties when violations occur.
The Office for Civil Rights: HIPAA's Primary Enforcer
The OCR operates with broad authority to investigate potential HIPAA violations. They receive thousands of complaints annually from patients who believe their privacy rights have been compromised. When a complaint is filed, the OCR follows a structured investigation process that can result in corrective action plans, monetary settlements, or formal enforcement actions.
The enforcement approach has evolved significantly since HIPAA's inception. Initially, the focus was primarily educational, helping covered entities understand their obligations. However, following the 2009 HITECH Act, enforcement became more aggressive, with increased penalties and mandatory breach notifications.
State Attorneys General: Additional Enforcement Layer
Beyond federal oversight, state attorneys general also play a crucial role in HIPAA enforcement. The HITECH Act granted state attorneys general the authority to file civil actions on behalf of residents who have been affected by HIPAA violations. This dual-level enforcement creates a comprehensive safety net for patient privacy protection.
State-level enforcement often focuses on large-scale breaches that affect significant numbers of residents within their jurisdiction. These cases frequently result in multi-million dollar settlements and serve as powerful deterrents for other healthcare organizations.
Criminal Enforcement Through the Department of Justice
While the OCR handles civil enforcement, criminal HIPAA violations fall under the jurisdiction of the Department of Justice (DOJ). Criminal charges typically involve cases where individuals knowingly obtain or disclose protected health information with intent to sell, transfer, or use the information for personal gain, commercial advantage, or malicious harm.
Criminal penalties can include fines up to $250,000 and imprisonment for up to 10 years, depending on the severity and intent of the violation. These harsh penalties underscore the serious nature of healthcare privacy breaches.
What HIPAA Covers
HIPAA's reach extends far beyond what many people realize. The law establishes national standards for protecting certain health information and applies to covered entities and their business associates.
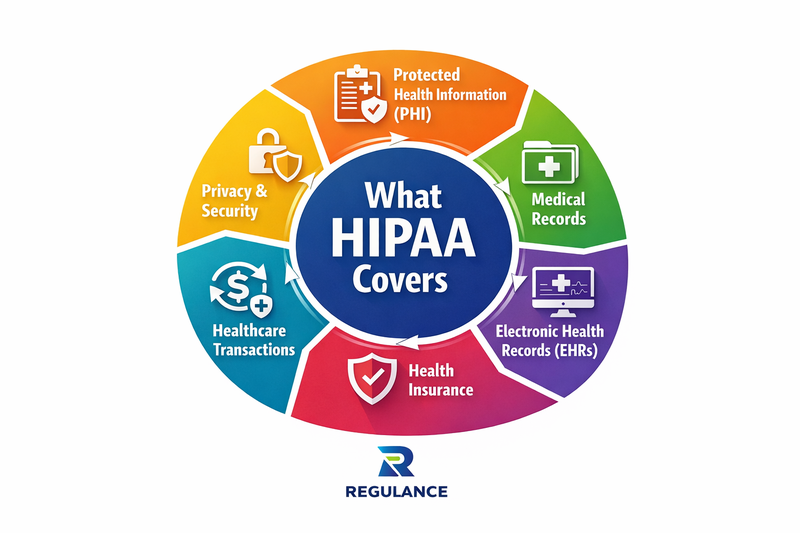
Covered Entities Under HIPAA
HIPAA applies to three main categories of covered entities: healthcare providers who conduct certain transactions electronically, health plans, and healthcare clearinghouses. This includes hospitals, clinics, psychologists, chiropractors, nursing homes, pharmacies, and dentists who transmit health information electronically.
Health plans encompass health insurance companies, HMOs, company health plans, and government programs like Medicare, Medicaid, and military and veterans' health programs. Healthcare clearinghouses are entities that process nonstandard health information they receive from another entity into a standard format.
Business Associates and HIPAA Compliance
The HITECH Act significantly expanded HIPAA's scope to include business associates, third-party vendors who handle PHI on behalf of covered entities. This includes cloud service providers, medical transcription companies, accounting firms, consultants, and legal firms that have access to protected health information.
Business associates must now comply directly with certain HIPAA provisions and can face penalties for violations. This expansion recognizes the modern healthcare ecosystem's interconnected nature, where patient information often flows through multiple organizations.
Protected Health Information (PHI)
HIPAA protects individually identifiable health information held or transmitted by covered entities and their business associates. This includes information in any form or media, whether electronic, paper, or oral. PHI encompasses medical records, billing information, and any other health information that could identify an individual.
The law establishes strict guidelines for how PHI can be used, disclosed, and protected. Patients have rights regarding their health information, including the right to access their records, request corrections, and receive notice of privacy practices.
Consequences of Violating HIPAA
HIPAA violations can result in severe consequences, both financial and reputational. The penalty structure is designed to reflect the severity of the violation and the covered entity's level of culpability.
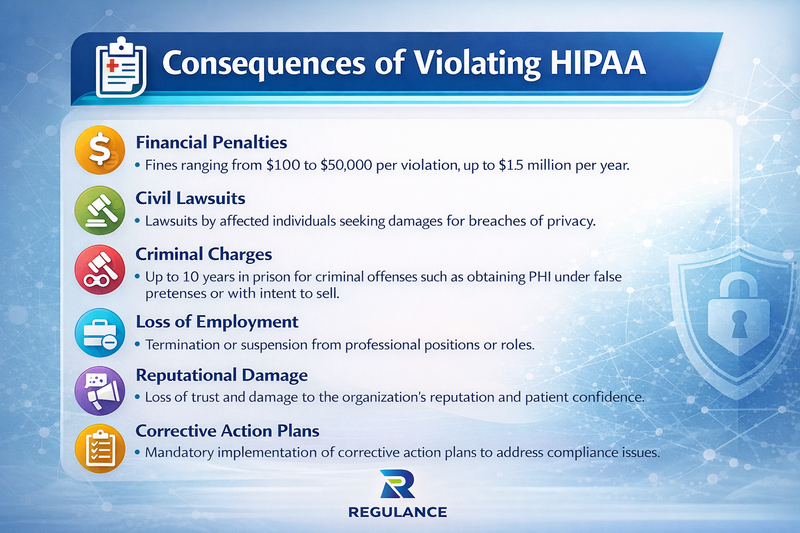
Civil Monetary Penalties
The OCR can impose civil monetary penalties ranging from $137 to $2,067,813 per violation, depending on the nature and extent of the violation and the covered entity's knowledge of the violation. The penalty tiers are structured as follows:
Violations where the entity was unaware and could not have realistically avoided the violation carry penalties of $137 to $68,928 per violation. For violations due to reasonable cause but not willful neglect, penalties range from $1,379 to $68,928 per violation.
More serious violations due to willful neglect that are corrected within 30 days result in penalties of $13,785 to $206,813 per violation. The most severe category willful neglect that is not corrected can result in penalties of $68,928 to $2,067,813 per violation.
Criminal Penalties and Prosecution
Criminal HIPAA violations are prosecuted by the Department of Justice and can result in both fines and imprisonment. The criminal penalty structure includes three tiers based on the intent and circumstances of the violation.
Violations committed under false pretenses can result in fines up to $100,000 and imprisonment for up to five years. The most serious violations, involving intent to sell, transfer, or use PHI for personal gain or malicious harm, can result in fines up to $250,000 and imprisonment for up to 10 years.
Reputational and Operational Consequences
Beyond financial penalties, HIPAA violations can cause lasting damage to an organization's reputation and operations. Public disclosure of breaches can erode patient trust, leading to decreased patient volume and revenue. Healthcare organizations may also face increased scrutiny from regulators, requiring additional resources for compliance monitoring and reporting.
Professional licensing boards may also take disciplinary action against individual healthcare providers involved in violations, potentially affecting their ability to practice. Insurance premiums for professional liability and cyber security coverage often increase following a breach, adding to the long-term financial impact.
Maintaining HIPAA Compliance
Maintaining HIPAA compliance requires a comprehensive, ongoing approach that encompasses policies, procedures, training, and technology. Organizations must implement administrative, physical, and technical safeguards to protect PHI effectively.
Administrative Safeguards
Administrative safeguards form the foundation of HIPAA compliance programs. These include conducting thorough risk assessments to identify potential vulnerabilities in PHI handling processes. Organizations must designate a HIPAA security officer responsible for developing and implementing security policies and procedures.
Employee training is crucial for maintaining compliance. All workforce members who handle PHI must receive comprehensive HIPAA training upon hire and regular refresher training thereafter. This training should cover privacy rights, proper handling of PHI, incident reporting procedures, and the consequences of violations.
Business associate agreements are essential when working with third-party vendors who may have access to PHI. These agreements must clearly outline each party's responsibilities for protecting PHI and include provisions for breach notification and compliance monitoring.
Physical Safeguards
Physical safeguards protect PHI in physical form and control access to facilities and equipment containing PHI. This includes implementing facility access controls such as locks, key cards, or biometric systems to restrict access to areas where PHI is stored or accessed.
Workstation security measures ensure that computers and other devices used to access PHI are properly secured. This includes positioning screens away from public view, using automatic screen locks, and ensuring proper disposal of devices containing PHI.
Device and media controls govern the receipt and removal of hardware and electronic media containing PHI. Organizations must maintain records of hardware and media movements and ensure proper data destruction when disposing of devices.
Technical Safeguards
Technical safeguards involve the technology and related policies that protect electronic PHI (ePHI) and control access to it. Access control measures ensure that only authorized individuals can access ePHI systems. This includes user identification systems, automatic logoffs, and role-based access controls.
Audit controls involve hardware, software, and procedural mechanisms that record and examine access to ePHI systems. These logs help detect unauthorized access attempts and monitor user activity within the system.
Transmission security ensures that ePHI is protected during electronic transmission. This includes encryption of data in transit, secure communication protocols, and protection against unauthorized access during transmission.
Automate HIPAA Compliance with Regulance AI
Modern healthcare organizations are increasingly turning to artificial intelligence and automated solutions to streamline HIPAA compliance efforts. Regulance AI represents a cutting-edge approach to compliance management that can significantly reduce the burden of manual compliance processes while improving accuracy and consistency.
AI-Powered Risk Assessment
Traditional HIPAA risk assessments are time-consuming, manual processes that may miss critical vulnerabilities. AI-powered solutions can continuously monitor systems and processes, identifying potential compliance gaps in real-time. These systems can analyze vast amounts of data to detect patterns that might indicate compliance risks, enabling proactive remediation.
Machine learning algorithms can learn from historical compliance data to predict areas of highest risk, allowing organizations to focus their resources where they're most needed. This predictive approach can prevent violations before they occur, reducing both financial and reputational risks.
Automated Policy Management
Maintaining current HIPAA policies and procedures is challenging, especially as regulations evolve and organizational processes change. AI-powered compliance platforms can automatically update policies based on regulatory changes and organizational modifications.
These systems can also track policy acknowledgments and training completion, ensuring all workforce members are current on their compliance obligations. Automated reminders and escalations help prevent gaps in training or policy compliance.
Intelligent Breach Detection
AI systems excel at detecting unusual patterns that might indicate a security breach or unauthorized access to PHI. By establishing baselines of normal user behavior, these systems can quickly identify deviations that warrant investigation.
Real-time monitoring capabilities enable immediate response to potential breaches, potentially minimizing the scope of exposure and reducing notification requirements. Early detection often means the difference between a minor compliance issue and a major regulatory violation.
Compliance Reporting and Documentation
Automated compliance platforms can generate comprehensive reports for regulatory audits and internal compliance monitoring. These systems maintain detailed audit trails that demonstrate ongoing compliance efforts and can quickly produce documentation required for OCR investigations.
Dashboards provide real-time visibility into compliance metrics, enabling leadership to make informed decisions about resource allocation and risk management. Automated reporting reduces the administrative burden on compliance staff while ensuring accuracy and completeness.
Integration with Existing Systems
Modern AI compliance solutions are designed to integrate seamlessly with existing healthcare IT infrastructure. This integration capability means organizations don't need to replace their current systems but can layer intelligent compliance monitoring and automation on top of existing investments.
API-based integrations enable real-time data sharing between compliance platforms and electronic health records, billing systems, and other healthcare applications. This comprehensive view of data flows is essential for effective HIPAA compliance monitoring.
Conclusion
HIPAA enforcement is a multi-layered system involving federal and state agencies, each playing crucial roles in protecting patient privacy. The Office for Civil Rights serves as the primary enforcer, conducting investigations and imposing penalties, while state attorneys general provide additional oversight, and the Department of Justice handles criminal violations.
Understanding what HIPAA covers is essential for all healthcare stakeholders. The law's scope extends to covered entities and business associates, protecting all forms of identifiable health information. The consequences of violations are severe, ranging from substantial financial penalties to criminal prosecution and lasting reputational damage.
Maintaining HIPAA compliance requires a comprehensive approach encompassing administrative, physical, and technical safeguards. Regular risk assessments, employee training, and robust policies and procedures form the foundation of effective compliance programs.
Learn who enforces HIPAA, how compliance works, and why protecting patient data is more critical than ever.